Oral & Maxillofacial Surgery
Oral and maxillofacial surgery is a dental specialty in the diagnosis and treatment of diseases, defects and injuries to the hard and soft tissues of the jaws, mouth, neck and face. Oral & Maxillofacial surgeons complete four to six years of training in addition to dental school.
Oral & maxillofacial surgeons perform a variety of surgeries, including:
- dental implants
- tooth extraction
- wisdom teeth extraction
- facial reconstruction
- cleft palate surgeries
- jaw misalignment treatment
- apicoectomy (root end surgery)
- biopsy and treatment of oral cancers, tumors and cysts
- sleep apnea treatment
- facial cosmetic surgery
Wisdom Teeth Extractions
Third molars, also called wisdom teeth, are the last teeth to surface, usually between ages 17-25. Most people have four wisdom teeth, some don’t have any, and in rare cases people have more than four. Your dentist observes your wisdom teeth with x-rays as part of regular examinations.
The Canadian Association of Oral & Maxillofacial Surgeons estimates that 85% of wisdom teeth will eventually require removal. Wisdom teeth are often impacted – not properly emerged through the gums, instead growing crooked or even completely sideways. Left untreated the impacted teeth can cause a host of problems including crowding or misalignment of the other teeth and jaw, headaches and infections. Even if not impacted, wisdom teeth can be difficult to clean and may require removal to reduce the risk of decay and infection.
The best time to remove wisdom teeth is when the patient is in their late teens-early 20’s, according to the Canadian Association of Oral & Maxillofacial Surgeons. Surgeries performed later in life can still be very effective, but healing may be slower, and the risk of complications slightly higher.
Wisdom teeth extraction is performed under local or general anesthetic and does not require an overnight stay.
Root Canal Therapy
 If the nerve within your tooth becomes infected, successful root canal treatment can keep you from losing the tooth while treating the infection before it causes health complications.
If the nerve within your tooth becomes infected, successful root canal treatment can keep you from losing the tooth while treating the infection before it causes health complications.
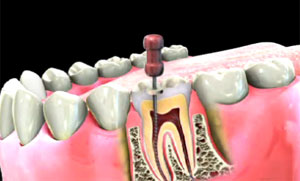
Properly performed, a root canal is no more uncomfortable than having a cavity filled, though the procedure is more complex. It is the removal of infected or dead pulp (the inner nerves and blood vessels) from inside the tooth, and the filling and sealing of the resulting space.
An infected (abscessed) tooth causes discomfort in the form of swelling and toothache. It can also cause severe health complications, because the bacteria from the infection can enter the bloodstream and travel to other parts of the body.
One way to treat the infection is to remove the tooth and disinfect the area. However, tooth loss creates a gap between surrounding teeth that often necessitates a dental implant or bridge. It is preferable to save the tooth if possible through root canal (endodontic) treatment.
The dentist begins by applying local anesthesia and isolating the area with a rubber dam. Then they drill an opening in the tooth to access the infected pulp, and remove it and clean the area with specialized tools. The dentist fills the root space with a filling material. Finally the dentist must seal the surface of the tooth with a crown to prevent further infection and restore the function and appearance of the tooth.
The root canal treatment is typically performed in one visit. A second visit may be required to complete the crown restoration.


 Wheel Chair Access
Wheel Chair Access